Suicide Prevention Month 2023
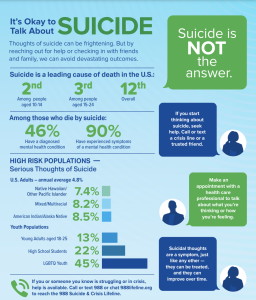
Each September, we mark Suicide Prevention Month and join the health community in opening up discussions and sharing information and resources about suicide prevention. Suicide is the 12th leading cause of death in the United States; the 2nd leading cause of death among people aged 10-14; and the 3rd leading cause of death among those aged 15-24 in the U.S. While these numbers are alarming and heartbreaking, we know that suicidal thoughts are treatable, and suicide is preventable with effective care. Below, NAMI information on warning signs and risk factors of suicide, and what you can do to support a suicidal loved one in a crisis. Together, we can work on suicide prevention and protect our loved ones and communities.
Facts
- 46% of people who die by suicide had a diagnosed mental health condition
- 90% of people who die by suicide may have experienced symptoms of a mental health condition, according to interviews with family, friends and medical professionals (also known as psychological autopsy)
- Annual prevalence of serious thoughts of suicide, high risk populations:
- Lesbian, gay and bisexual youth are nearly 4x more likely to attempt suicide than straight youth
- 79% of people who die by suicide are male
- Transgender adults are nearly 9x more likely to attempt suicide at some point in their lifetime compared to the general population
- Suicide is the leading cause of death for people held in local jails. (Facts from NAMI.)
Warning Signs
- Increased alcohol and drug use
- Aggressive behavior
- Withdrawal from friends, family and community
- Dramatic mood swings
- Impulsive or reckless behavior
Suicidal behaviors are a psychiatric emergency. If you or a loved one starts to take any of these steps, seek immediate help from a health care provider or call 911:
- Collecting and saving pills or buying a weapon
- Giving away possessions
- Tying up loose ends, like organizing personal papers or paying off debts
- Saying goodbye to friends and family
If you are unsure, a licensed mental health professional can help assess. Know the sign:
Risk Factors
Research has found that 46% of people who die by suicide had a known mental health condition. Several other things may put a person at risk of suicide, including:
- A family history of suicide
- Substance abuse. Drugs can create mental highs and lows that worsen suicidal thoughts.
- Intoxication. More than 1 in 3 people who die from suicide are under the influence of alcohol at the time of death.
- Access to firearms
- A serious or chronic medical illness
- Gender. Although more women than men attempt suicide, men are nearly 4 times more likely to die by suicide.
- A history of trauma or abuse
- Prolonged stress
- A recent tragedy or loss
Help in a Crisis for You or a Loved One
There is always help and hope. We want to make sure that you get the help you need.
Please know that you are not alone. There are many (free) resources (discussion groups, social media platforms, crisis hotlines, emotional support warmlines, etc.) where you can reach out to either talk with someone confidentially about your feelings and/or share and learn from others. And with psychotherapeutic and psychiatric treatments available, there is no reason for you to continue to suffer and be prevented from successful recovery to live a full and content life.
- You can also contact the 988 Mental Health and Suicide Crisis Line, which has trained and compassionate crisis workers available 24/7 to talk with you about your feelings and work with you to develop a plan for staying safe.
- NAMI has a warmline available Monday through Friday, 7 am to 7 pm PT. Call1-800-950-NAMI (6264), text “HelpLine” to 62640 or email at helpline@nami.org
- Our NAMI WLA affiliate also has a warmline weekdays during business hours.
- If you or someone you know is imminent danger of hurting themselves or someone else, please do not hesitate to take them to the nearest emergency room or call 911 for help.
How to Talk About Suicide
How and when we talk about suicide can save lives. Here are some DOs and DON’Ts. Do: Say he died by suicide or he ended his/her/their life. Don’t: Say he/she/they committed suicide. We do not want to criminalize mental health crises. Do: Say it was an attempted suicide. Don’t: Say it was an unsuccessful suicide. We don’t want to make someone in a mental health crisis feel worse. Do: Speak to youth about suicide. In recent years, rates of death by suicide and suicidal thinking have increased in young people. Asking about suicide may be a relief for people of all ages. If your child has a mental health condition, it’s important to check-in with them about suicidal thoughts. Don’t: Be afraid to speak about suicide with youth. Many parents and caregivers are wary of asking a child if they have suicidal thoughts, intentions or plans. They may be afraid that starting the conversation may cause suicidal behavior, but this connection has proven to be false. Do: Speak to loved ones who struggle with suicidal ideation openly and with compassion. Let them know that they can talk with you about what they’re going through. Make sure that you adopt an open and compassionate mindset when they’re talking. Try active listening techniques such as reflecting their feelings and summarizing their thoughts. This can help your loved one feel heard and validated. Don’t: Argue, threaten, or raise your voice. Don’t debate whether suicide is right or wrong. Don’t try to disprove any negative statements they make (“Your life isn’t that bad!”). Do: Know when to talk about suicide. Listen for when a loved one is expressing suicidal thoughts, either through explicit statements such as “I want to die” or more vague statements such as “I don’t want to be here anymore.” Don’t: Agree to keep a youth’s suicidal thoughts secret. Even if they don’t want anyone else to know, it is important to get help if you are truly afraid that they will hurt themselves. Getting help could involve letting their family know about the crisis, unless you have a clear reason to think that will make things worse (for example, they have shared that their parents do not support them or they have been mistreated or experienced rejection at home). If you in a school environment, let the crisis team, residence life staff or counseling service know you are worried about your friend. Do: Gently suggest professional help. Let loved ones experiencing suicidal thoughts know that mental health professionals are trained to help people understand their feelings and improve mental wellness and resiliency. Psychotherapy, like cognitive behavioral therapy and dialectical behavior therapy, can help a person with thoughts of suicide recognize ineffective patterns of thinking and behavior, validate their feelings and learn coping skills. Suicidal thoughts are a symptom, just like any other — they can be treated, and they can improve over time. Suicide is not the answer. There is hope. Do: Offer to get help. Calmly ask simple and direct questions, like “Can I help you call your psychiatrist or the crisis line?” If there are multiple people around, have one person speak at a time. Don’t: Be afraid to ask direct questions about suicide. It is okay to express support and concern and ask if a person has a suicide plan. You can directly ask, “Do you have a plan for how you would kill yourself?” More: How to Talk (and Listen To) Someone Experiencing Suicidal Thoughts (NAMI blog post) Do: Express support and concern and tell the person you are care about them. Don’t: Argue, threaten or raise your voice.